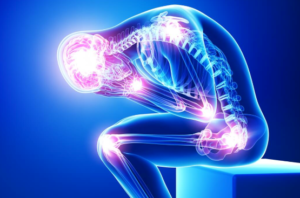
Arthritis refers to a range of conditions characterized by joint inflammation. While often associated with aging, arthritis affects individuals of all ages, including children. The condition primarily targets the joints, such as in the knees, hips, and hands. The inflammation can lead to pain, stiffness, and swelling, which may limit a person’s ability to perform daily activities.
What Effect Does Arthritis Have?
Arthritis is fundamentally a condition of joint inflammation. In a healthy joint, cartilage cushions the ends of the bones, allowing for smooth, painless movement. When arthritis develops, this cartilage can begin to break down. As the cartilage wears away, the bones may rub directly against each other, causing pain, swelling, and reduced range of motion. The body’s inflammatory response may also damage the joint and surrounding tissues.
The impact of arthritis extends beyond physical discomfort. Persistent pain and stiffness can make simple tasks very difficult. This may lead to a reduction in physical activity, which may contribute to other health issues such as weight gain and decreased muscle strength. The unpredictability of symptoms, with periods of flare-ups and remission, can also be challenging to manage, affecting a person’s daily routine and long-term plans. Arthritis’s overall effect on quality of life may be substantial, influencing a person’s ability to live fully and actively.
What Causes It?
The causes of arthritis vary depending on the specific type. The two most common forms are osteoarthritis and rheumatoid arthritis, each with distinct origins. Osteoarthritis (OA) is the most prevalent type. It is often described as a “wear and tear” condition. The protective cartilage on the ends of your bones can deteriorate over time. This process is accelerated by factors such as age, joint injury, and repetitive stress on the joints.
Rheumatoid arthritis (RA) is an autoimmune disorder. This means the body’s immune system mistakenly attacks its own tissues. In the case of RA, the immune system targets the synovium, which is the lining of the membranes that surround the joints. This attack can eventually destroy the cartilage and bone within the joint.
How Is It Treated?
Management of arthritis focuses on alleviating symptoms, improving joint function, and slowing the progression of the condition. Treatment plans are tailored to the individual and based on the type and severity of arthritis. A multidisciplinary approach is often employed.
Lifestyle modifications are a foundational component of treatment. Physical activity, particularly low-impact exercises like walking and cycling, can help improve range of motion and strengthen the muscles around the joints. Maintaining a healthy weight reduces stress on weight-bearing joints such as the knees, hips, and spine.
Medications are also commonly used. Over-the-counter pain relievers and anti-inflammatory drugs may be recommended for mild to moderate pain. For RA, specific medications known as disease-modifying antirheumatic drugs (DMARDs) and biologics may be prescribed to suppress the immune system’s attack on the joints.
Physical therapy provides significant benefits. A physical therapist can design a personalized exercise program to improve strength and flexibility. In cases where joint damage is severe and conservative treatments are no longer effective, surgical intervention may be an option. Procedures like joint replacement can restore function and relieve pain.
Confer With a Medical Specialist
Living with arthritis presents many challenges, but various strategies exist to manage its impact on your life. Since arthritis encompasses a wide array of conditions with different causes and progression patterns, obtaining an accurate diagnosis is a necessary step. A medical professional can properly evaluate your symptoms, identify the specific type of arthritis, and enact a comprehensive management plan tailored to your unique circumstances.