Spider veins are small, visible blood vessels that form web-like patterns beneath the skin, most often on the legs and face. While not linked to severe medical complications, they may create physical symptoms such as aching or burning and may be a source of distress for many individuals. Learning about the development of these veins, their characteristics, and available treatment methods supports individuals in addressing both appearance and physical symptoms.
What Are Spider Veins?
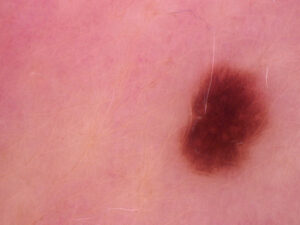
Spider veins are blood vessels that appear red, blue, or purple. These veins are close to the skin’s surface and take on a web- or branch-like configuration. The name comes from their resemblance to a spider’s web radiating outward. These veins differ from varicose veins, which are thicker, raised, and often more pronounced. Spider veins stay flat and are not typically raised above the skin. They develop when small blood vessels near the surface become dilated, causing blood to pool and form visible clusters.
Common locations include the thighs, calves, ankles, and knees. The progression may be gradual, with spider veins becoming more apparent over time. In some individuals, these veins occur without symptoms. For others, they may result in mild swelling, aching, or itching sensations.
What Causes Them?
Multiple factors influence the formation of spider veins. Family history is a primary contributor, as a genetic predisposition can affect vein wall structure and valve function. People with close relatives who have spider or varicose veins are at greater risk of developing them.
Hormonal influences are also a factor. These veins are observed more commonly in women, particularly during events such as pregnancy and menopause or when taking hormone replacement therapies or contraceptive pills. The hormone estrogen may weaken vein walls, leading to dilation.
As people age, vein walls can lose flexibility, and valves may function less effectively, allowing blood to pool in the vessels. Jobs or situations requiring prolonged standing or sitting put added strain on leg veins by impairing blood flow. Other risk factors include excess body weight and sun exposure.
How Are They Treated?
Treatment for spider veins can be procedural or supportive. This will depend on the extent and location of the veins, as well as the patient’s health history and preferences. Medical evaluation determines the most suitable approach.
Sclerotherapy is widely used, especially for leg veins. In this in-office procedure, a solution is injected into the affected vessel, causing it to close and be absorbed by the body. Several sessions may be needed based on the amount and size of veins. Laser therapy can be used for small leg vessels. Focused light energy targets veins, causing them to gradually fade. Laser procedures are non-invasive and can be suited for individuals who wish to avoid injections.
Supportive measures help manage symptoms and may limit further progression. Medical-grade compression stockings apply external pressure to the legs, supporting vein function and helping reduce pooling of blood in superficial veins. Physical activity can promote better blood circulation, supporting vascular health. Elevating the legs while resting and maintaining movement during extended periods of sitting or standing also supports venous circulation.
Speak With a Vascular Specialist
Understanding the factors behind spider veins’ development and available treatments allows individuals to address symptoms with current, evidence-based approaches. A consultation with a vascular specialist enables an informed evaluation of your vein health and facilitates a path toward treatment. Specialists can differentiate this condition from other issues and recommend treatment or symptom management strategies based on your specific needs.